#037
Training nurses to work
in transformative oncology
care settings
Yoshie Murakami
Japanese Color:Tsutsuji-iro
#037
Yoshie Murakami
Japanese Color:Tsutsuji-iro
MOVIE

Professor
Faculty of Nursing and Medical Care
Advances in genomic analysis are bringing rapid and widespread progress in a branch of medicine known as cancer genomics, allowing more patients to receive treatment tailored to the types of genetic mutations present in the cancer cells growing in their body. This, in turn, is changing the requirements that nurses are expected to meet in terms of their knowledge and care. Professor Yoshie Murakami has been a pioneer in the field of cancer genetic counseling in Japan since its inception, and has incorporated psycho-oncology nursing into her counseling practice. She is committed to research and education for the training of nurses in the era of genomic medicine, utilizing her experience.
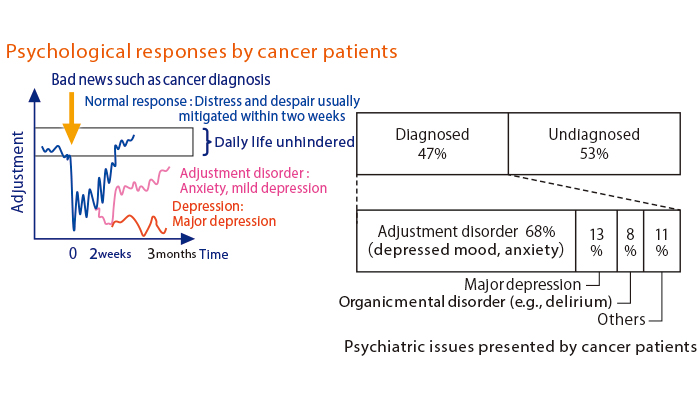
Psycho-oncology is a new field of study established in the 1980s. It is a combination of psychiatry and psychology and oncology, which is the study of cancer.
Most nurses have experienced a situation in which a cancer patient reveals a desire to die. In such cases, we nurses perform a wholistic assessment of the patient by listening to their expressed wishes and thinking, and provide nursing care accordingly. When a patient expresses a death wish, we tend to suspect an underlying mental problem, but our first priority is to assess their physical symptoms and check for any physical pain. This approach prevents us from missing any physical suffering of a degree that would lead them to prefer death. In addition, nurses also carefully look into the patient’s general circumstances by conducting a comprehensive assessment of their psychiatric symptoms as well as any socioeconomic, psychological, and existential issues.
Nurses also leverage diverse skills in communicating with patients. One of them is known as SPIKES—an abbreviation for setting, perception, invitation, knowledge, empathy, and strategy and summary. SPIKES provides a framework for breaking bad news to patients in a supportive way.
Nurses involved in psycho-oncology are responsible for providing care by applying such skills at every step of a cancer patient’s journey, from the point of announcing the cancer diagnosis, through the treatment phase, and to the end-of-life stage.
Alongside psycho-oncology, “cancer genomics and nursing care” is also a substantial research theme. Thanks to the recent progress achieved in genomics research, more people with cancer are able to choose personalized oncology therapies and drugs that distinctly address the types of genetic mutations exhibited by their cancer.
In 2019, cancer genomic medicine core base hospitals and other medical institutions across Japan started performing the cancer gene panel testing covered by the national health insurance system. The testing allows patients with limited treatment options to have dozens to several hundreds of their genes exhaustively examined in an effort to identify clinical trial or unapproved drugs that may work for them. For patients who have exhausted all standard treatment options, the testing offers a last ray of hope. Not surprisingly, these patients feel deeply disappointed in the event they fail to meet the testing criteria or no recommendable drug is identified as a result of the testing. Oncology nurses support patients and their families from the pre-testing phase, all the while prepared for such unfortunate possibilities.
Furthermore, when the testing reveals genetic mutations related to the onset of a hereditary cancer, the patient and their family members may exhibit an intense reaction, sometimes causing an upset in the clinical setting. This is partly due to a lack of experience and skills on the part of healthcare professionals to communicate the possibility of inherited tumors in a supportive manner. Recognizing the need to foster professionals who can engage in cancer genomics medical care without prejudice or discomfort, we have been developing special training programs for oncology nurses.

It was an encounter with a familial adenomatous polyposis patient that aroused my interest in cancer genomics medicine when I was pursuing my master’s degree. The illness was an inherited condition that led to the formation of more than 100 polyps in the large intestine. At the time, the standard treatment was to remove the entire large intestine before the polyps developed into cancer.
I was shocked to learn about the patient’s delicate challenges concerning defecation, which prompted me to think about what I could do to help as a nurse. On learning that the condition was hereditary, I also felt a pressing need to support the patient and family in other aspects of their life, in addition to their medical needs.
There being hardly any doctors or nurses who worked with hereditary tumors back then, I also felt the urge to raise awareness. Coincidentally, the Japanese Society of Familial Tumor (the current Japanese Society for Hereditary Tumors) hosted the First Familial Tumor Counselor Training Seminar in 1998 and I jumped at the opportunity to participate. The following year, I joined the organizers to create a role-playing scenario for genetic counseling, and have been engaged in various related initiatives ever since.
Going forward, genomic information will play a greater role in diagnosing illnesses and making treatment decisions in wider areas of healthcare including cancer. I intend to teach the basics of genomics and genetic literacy to undergraduate students, who will be sustaining the healthcare services of the future.


Yoshie Murakami
Graduated from the teacher training course, Faculty of Education (Nursing), Hirosaki University in 1990. Completed the master’s course at the College of Nursing Art and Science, University of Hyogo in 1999. After working at the National Cancer Center Research Institute and others, acquired a doctoral degree in nursing science from St. Luke’s College of Nursing Graduate School in 2008. Appointed as professor of the Faculty of Nursing, Toho University in 2012. In current position since 2024. Received the Society Award from the Japan Psycho-Oncology Society in 2016. Received the Toho University Education Award in 2017.

2023.Nov ISSUE